
PARTIAL-LOAD EMPLOYEE BENEFITS
PLEASE NOTE: Although every effort has been made to ensure the posted information is accurate and up-to-date, consult your printed copy of the Collective Agreement or Benefits Booklet before taking any action. All external links open in a new tab.
Section 1 - General Information
About this booklet
This booklet has been developed for you and your family by individuals currently on the Academic Joint Insurance Committee (JIC) who represent the Ontario Public Service Employees Union (OPSEU), the Colleges of Applied Arts and Technology (CAAT), the College Employer Council (CEC), and representatives from the Insurance Company, Sun Life.
Benefits for Partial-Load employees were established under the Academic Pay Equity Plan as required by the ‘Pay Equity Act, (1987)’. The effective date for participation in benefits was July 1, 1990.
The information contained in this booklet will not in any way diminish current benefit levels in effect as of the date of issue.
The information in this booklet is important to you and should be kept in a safe place. It describes all group insurance benefits available to you, explains your entitlements and various administrative issues relating to the Group Insurance Benefit Program. For confirmation of the specific benefit coverage you have elected, please refer to your copy of your Group Insurance Positive Enrolment Form or contact your College s Benefits Administrator.
It is important to note that this booklet is only a summary of your group contract. It is not a legal document. If there are any discrepancies between the group contract and the information in this booklet, the group contract will take priority and the Insurance Company will follow the group contract when making a decision to pay a claim.
Benefits described in the booklet are applicable only if you and your Dependent(s) are insured according to the records maintained for the group contract. If you have any questions about the information in this employee benefits booklet, or if you need additional information about your group benefits, please contact your College s Benefits Administrator or Union Local Representative.
About the Group Insurance Benefits Program
The group insurance benefit program and the cost-sharing arrangements provided to the CAAT Academic Partial-Load Employee Group are a result of negotiations and are set out in the Academic Staff Collective Agreement.
Section 2 - Roles & Responsibilities
College Employer Council
(Contract Holder)
The CEC is the Contract Holder on behalf of the Colleges, and is responsible to ensure that the terms of the group contract are adhered to by the Insurance Company and the Colleges.
About the Joint Insurance Committee (JIC)
The Academic JIC consisting of representatives of OPSEU, CAAT and CEC has been established under the Terms of Reference in the Academic Collective Agreement. The committee meets on a regular basis to discuss group insurance benefits matters. The duties of the Committee include the review of contentious claims and recommendations thereon, when such claim problems have not been resolved through the existing administrative procedures.
Colleges
(Administrators)
The Colleges of Applied Arts and Technology are responsible to:
- maintain all records regarding an employee s coverage.
- ensure the group contracts are adhered to.
- communicate the provisions of the group contract to employees.
Each College has a designated individual(s) in the Human Resources Division and/or Payroll Services who is responsible for the group insurance benefit program.
OPSEU
(the employee’s representative)
OPSEU is responsible to:
- represent employees covered by the Academic Collective Agreement on matters relating to group insurance benefits.
- educate members about benefits.
- communicate with the Contract Holder (CEC) on matters relating to the group insurance benefits.
- participate with the College Employer Council in discussions about Group Insurance Benefit issues through the Joint Insurance Committee (JIC) in accordance with the Terms of Reference of the Academic JIC as outlined in the Collective Agreement.
Sun Life
(Insurance Company)
The Insurance Company is responsible to adjudicate and pay claims in accordance with the provisions in the group contract between Sun Life and the College Employer Council on behalf of the Colleges.
Employee
You are responsible to:
- know what your benefits are.
- follow the claims submission processes, providing the information requested.
- be an educated consumer.
- keep the Human Resources Department at your College informed about changes that may affect the status of your benefits.
Section 3 - Definitions
Accident
An accident is a bodily injury that occurs solely as a direct result of a violent, sudden and unexpected action from an outside source.
Actively At Work
You are considered to be ‘actively at work’ if you are performing all the usual and customary duties of the job with the College for the scheduled number of hours.
Appropriate Treatment
Appropriate treatment is defined as any treatment that is performed and prescribed by a doctor or, when Sun Life believes it is necessary, by a medical specialist. It must be the usual and reasonable treatment for the condition and must be provided as frequently as is usually required by the condition. It must not be limited solely to examinations or testing.
Benefit Year & Calendar Year
January 1 to December 31.
Dentist
A person who is currently licensed to practise dentistry by the governmental authority having jurisdiction over the licensing and practising of dentistry, and who is operating within the scope of the issued licence. The definition usually includes licensed dental hygienists, dental assistants or denturists, etc.
Dependent(s)
Who qualifies as your dependent:
The dependent must be your spouse or your child and a resident of Canada or the United States.
Spouse/Partner
Spouse means:
- Your spouse by marriage or under any other formal unionrecognized by law
- Your partner of either gender who is publicly represented as yourspouse with whom you have cohabited for one full year (12continuous months) or,
- If you are the natural or adoptive parents of a child as defined inthe Family Law Act 1990 (Ontario)
Note: For group insurance purposes, your spouse/partner will cease to meet the definition of a person qualified as your dependent upon the earlier of:
- The date you have entered into a Separation Agreement withyour spouse/partner; or
- Without a Separation Agreement , having lived separate andapart from your spouse for not less than 12 months.
You can cover only one spouse at any time
Dependent Child(ren)
Your children and your spouse s children (other than foster children) are eligible dependents if they are not married on in any other formal union recognized by law, and under age 21.
A child who is a full-time student attending an educational institution recognized under the Income Tax Act (Canada) is also considered an eligible dependent until the age of 25 as long as the child is entirely dependent on you for financial support.
If a child becomes disabled before the limiting age, we will continue coverage as long as:
- The child is incapable of financial self-support because of aphysical or mental disability, and
- The child depends on you for financial support, and is notmarried nor in any other formal union recognized by law
In these cases, you must notify your College s Benefits Administrator within 31 days of the date the child attains the limiting age. In addition, a Disabled Child Coverage form must be completed and sent to Sun Life within 6 months of the date the child attains the limiting age. Your employer can give you more information about this.
Doctor
A doctor is a physician or surgeon who is licensed to practise medicine where that practice is located.
Eligibility Requirements
Conditions that must be satisfied in order to participate in the Plan, and obtain a benefit.
Partial-Load Employee
You are employed by the College on a Partial-Load basis in accordance with the terms of the Academic Collective Agreement.
Hospital
Hospital is defined as a legally operated institution which is primarily engaged in providing, for compensation from its patients, medical, diagnostic and surgical facilities for the care and treatment of sick and injured persons on an in-patient basis, and provides such facilities under the supervision of a staff of doctors with a 24 hour a day nursing service by registered nurses.
Notwithstanding the above, hospital shall mean a legally operated institution in which a person establishes, to the satisfaction of Sun Life, that such confinement was for active treatment that would normally be found in a general hospital.
In no event will that part of an institution which operates as a home for the aged, rest home, nursing home, chronic care facility or a place for the care and treatment of drug addicts or alcoholics be considered a hospital for the purpose of this contract.
Facilities and services that are not covered
The Plan does not cover the facility nor the services provided in a nursing home, rest home, home for the aged or chronically ill, sanatorium, convalescent hospital or a facility for treating alcohol or drug abuse or beds set aside for any of these purposes in a hospital.
Palliative Care
Services for palliative care provided at a hospital, as defined under Regulation 964 under the Public Hospitals Act, R.S.O. 1990, c.P-40 are covered by the Extended Health Care Plan.
Services for palliative care provided at Casey House or any other hospice which is approved for hospital purposes pursuant to an Order-in-Council under the Public Hospitals Act are covered by the Extended Health Care Plan.
Illness
An illness is a bodily injury, disease, mental infirmity, sickness or the consequences of surgery needed to donate a body part to another person.
Incurred Expense
You incur an expense on the date the service is received or the supplies are purchased or rented.
Reasonable and Customary Expenses
Standard medically approved treatments and procedures which are normally applied in the treatment of a particular illness or condition and are provided at costs equivalent to the normal charges for such treatment in the location where such treatment is provided.
Survivor(s)
Eligible Dependent(s) of an employee who becomes deceased while employed by the College provided the employee was participating in the group insurance benefits at the time of his or her death. Refer to Section 10 for further details.
Section 4 - Categories of Benefits
Basic Benefit
All Partial-Load employees shall participate in the following benefit. However, if you have Extended Health Care coverage through your spouse’s group insurance plan you may elect in writing to wave this coverage:
- Extended Health Care
Premiums
| Benefits | College Pays | You Pay |
|---|---|---|
| Extended Health Care | College Pays 100% | You Pay 0% |
Optional Benefits
You may elect to participate in the following benefits:
- Basic Life Insurance
- Accidental Death and Dismemberment Insurance
- Supplementary Life Insurance
- Employee Pay-All Life Insurance
- Dependent Life Insurance
- Vision Care
- Hearing Care
- Dental Care
- Critical Illness Insurance
Premiums
| Benefits | College Pays | You Pay |
|---|---|---|
| Basic Life Insurance | Basic Life Insurance College Pays 0% | Basic Life Insurance You Pay 100% |
| AD & D Insurance | AD & D Insurance College Pays 0% | AD & D Insurance You Pay 100% |
| Supplementary Life Insurance | Supplementary Life Insurance College Pays 0% | Supplementary Life Insurance You Pay 100% |
| Employee Pay-All Life Insurance | Employee Pay-All Life Insurance College Pays 0% | Employee Pay-All Life Insurance You Pay 100% |
| Dependent Life Insurance | Dependent Life Insurance College Pays 0% | Dependent Life Insurance You Pay 100% |
| Vision Care | Vision Care College Pays 0% | Vision Care You Pay 100% |
| Hearing Care | Hearing Care College Pays 0% | Hearing Care You Pay 100% |
| Dental Care | Dental Care College Pays 0% | Dental Care You Pay 100% |
| Critical Illness Insurance | Critical Illness Insurance College Pays 0% | Critical Illness Insurance You Pay 100% |
Premium Deductions
In addition to the cost of the benefits, if you are a resident of Ontario or a resident of Quebec, provincial retail sales tax is applied to the actual premium and must be paid by you and the College. The College s Benefits Administrator will provide the premium deduction information to you at the time of enrolment.
Section 5 - When Coverage Begins
New Employee
The waiting period for a new employee under your group contract is indicated on the following chart. For purposes of your group insurance benefits, you are considered a new employee under your first partial-load contract or if there is a break of more than 6 months between partial-load contracts.
| BENEFIT | WAITING PERIOD |
|---|---|
| Basic Life Insurance | Basic Life Insurance Waiting Period: First of the month following the completion of one calendar month of partial-load employment. |
| Accidental Death & Dismemberment Insurance | Accidental Death & Dismemberment Insurance Waiting Period: First of the month following the completion of one calendar month of partial-load employment. |
| Supplementary Life Insurance | Supplementary Life Insurance Waiting Period: First of the month following the completion of one calendar month of partial-load employment. |
| Employee Pay-All Life Insurance | Employee Pay-All Life Insurance Waiting Period: First of the month following the completion of one calendar month of partial-load employment. |
| Dependent Basic Life Insurance | Dependent Basic Life Insurance Waiting Period: First of the month following the completion of one calendar month of partial-load employment. |
| Extended Health Care (including Vision and Hearing Care) | Extended Health Care (including Vision and Hearing Care) Waiting Period: First of the month following the completion of one calendar month of partial-load employment. |
| Dental Care | Dental Care Waiting Period: First of the month following the completion of six calendar months of partial-load employment. |
| Critical Illness Insurance | Critical Illness Insurance Waiting Period: On completion of one calendar month of partial-load employment. |
Bridging Benefits and Waiting Period
If you were participating in a benefit and have completed your initial waiting period and you become re-employed with the College within 6 months of the end of any partial-load contract, waiting periods for these benefits will be waived and coverage will be effective from the first day of the new partial-load contract.
Optional benefits once declined/not elected are not available unless more than 6 months have expired between partial-load contracts. Where more than 6 months have expired between partial-load contracts, you will have to complete a new enrolment form and elect the coverage you wish. The appropriate waiting periods must be served on all the benefits you elect (see above table).
Coverage begins
Your coverage begins the first day following the completion of the waiting periods provided you are ‘actively at work’ on the date your coverage becomes effective. In the event you are absent on that date, you will qualify on the day you return to ‘active work’. For Critical Illness coverage, refer to Section 18.
You must be actively at work on the date you qualify for the insurance but if you are absent on that date, you will qualify on the day you return to active work.
If for any reason, you stop being actively at work, you should contact the Benefits Administrator at your College to determine the status of your benefits.
In the event benefit improvements for Life Insurance are negotiated, you must be actively at work on the date improvements to the Life insurance are effective in order to qualify for such improvements. If you are absent on that date, you will qualify on the date you return to active work.
Dependent(s)
Coverage for your Dependents begins on the latest of:
- the date you become eligible, if they are your Dependents on that date,
- the date they first become your Dependents after the effective date of your coverage, if your request for coverage is received by the College within 31 days, or
- for Life Insurance, on the date of approval by Sun Life if your request for coverage is received later than 31 days after they first become your Dependents.
- for Vision Care, Hearing Care and Dental Care, if the request is received after 31 days, coverage is no longer available until there is a 6 month break between your partial-load contracts.
- for a Dependent, other than a newborn child, who is hospitalized, coverage will begin when the dependent is discharged from hospital.
Section 6 - Enrolment
Enrolment Form
At the time you commence employment, the Benefits Administrator at your College will provide you with information about your Group Insurance Benefit options.
You will be required to complete and sign a detailed enrolment form which collects the necessary information about yourself and your Dependent(s) (if applicable), in order for the College to administer the Group Insurance Benefit Program, and for Sun Life to adjudicate and process claims. It is important that you read this form, fully answer the questions, sign and date the form where required and return it to your Benefits Administrator no later than 31 days after you become eligible for the Extended Health Care coverage without jeopardizing your entitlement to coverage.
This enrolment form also contains information relating to the completion date of your waiting period and the effective date of your benefits coverage.
You will be enrolled in the mandatory and optional benefits following completion of the appropriate waiting periods.
Your Certificate Number
Your College will assign you a certificate number that will be used to set up your benefit information and which you can use to generate an identification card on line in the event you need to produce proof that you have benefit coverage. This certificate number will be a unique number and will contain a code to identify your employee group, your College and your file. This is necessary in order for Sun Life to process your claims and for you to access your claims information.
Confidentiality
Your privacy is respected and the personal information collected is held between your College and Sun Life in the strictest confidence. At Sun Life Financial, access to your personal information is restricted to the persons outlined in the Respecting Your Privacy clause at the end of this booklet.
Updating your Records
To ensure that your benefit coverage is kept up-to-date, it is important that you report any of the following changes to your Benefits Administrator at the College:
- change of name.
- change of beneficiary.
- addition of a spouse/partner and/or dependent child.
- change in marital status.
- death of a spouse/partner and/or dependent child.
Accessing your records
Where required by legislation, for insured benefits, you may obtain copies of the following documents:
- your enrolment form or application for insurance.
- any written statements or other record, not otherwise part of the application, that you provided to Sun Life as evidence of insurability.
- with reasonable notice, the contract. The first copy will be provided at no cost to you but a fee may be charged for subsequent copies.
All requests for copies of documents should be directed to one of the following sources:
- Sun Life’s website at www.mysunlife.ca.
- Sun Life’s Customer Care Centre by calling toll-free at 1-800-361-6212.
Section 7 - Changing Benefit Coverage
Changes affecting your coverage
Changes in employment and personal status may affect your benefit coverage. It is important for you to contact your Benefits Administrator to discuss your benefit coverage prior to the effective date of an employment status change or within 31 days following a personal status change.
Personal status changes and Extended Health and Dental Care benefits
You may change your Extended Health, Vision, Hearing, and Dental Care coverage from single to family or vice-versa under the following special circumstances:
- if there is a change in your marital status.
- if you gain or lose a dependent.
To change your coverage, you must notify the Human Resources Department within 31 days of when the change takes place.
To determine when a spouse/partner will cease to qualify as a Dependent please see Section 3, Definitions Spouse/Partner.
To add or increase Life Insurance coverage
In the event you wish to add, or change the amount of your Optional Life Insurance, or obtain Life Insurance for a newly acquired Dependent, you may do so without a medical examination or other evidence of insurability provided you are actively at work and you apply for the Life Insurance coverage for you or your Dependent within 31 days of the date you acquire a Dependent or an additional Dependent
Proof of good health
To increase your Life Insurance or obtain Dependent Life Insurance at any time other than referenced above, you will be required to submit proof of good health via a Health Questionnaire Form obtained from the College’s Benefits Administrator.
If coverage previously declined
In the event you have previously applied for and been declined for additional Life Insurance coverage, the 31 days provision referenced above is not applicable. You will be required to continue to submit proof of good health to Sun Life, and depending on your individual situation, may never be eligible for this coverage.
Effective date of coverage
- if proof of good health is required, the change cannot take effect until Sun Life approves your application.
- if you are not actively working when the change occurs or when Sun Life approves proof of good health, the change cannot take effect before you return to active work.
- if a Dependent, other than a newborn child, is hospitalized on the date when the change occurs, the change in the Dependent’s coverage cannot take effect before the Dependent is discharged from hospital.
Section 8 - Bridging Group Insurance Benefits
What is Bridging?
Bridging refers to your entitlement to maintain benefit coverage between your current partial-load contract and re-employment under a subsequent partial-load contract.
What happens to my benefits during the bridging period?
You may continue the benefits at the end of your contract:
- until your next contract if you have a written contract of future partial-load employment, or
- if you have been granted a leave of absence by the College as per Articles 21, 22 of the Collective Agreement for a maximum period of 24 consecutive months.
Who pays the premium?
If you pay 100% of the cost of premiums, benefits will continue.
How are the waiting periods affected?
There is no waiting period on benefits that you have bridged or if you are rehired within six months as a partial-load employee.
A waiting period is applicable again if more than 6 months has elapsed between partial-load contracts.
Section 9 - Termination of Coverage
When coverage ends
For Active Employees
Benefit coverage will end on the earliest of the following dates:
- the end of the month in which your employment terminates.
- the end of the month in which you retire.
- the date the group contract is no longer in force.
- the end of the period for which the premium is paid for your insurance.
- the date you die.
- for Supplemental Life, Employee Pay-All Life and Dependent Life, the end of the month in which you attain age 65, but no later than August 31st following your 65th birthday if you are actively at work.
- for Critical Illness, see Section 18.
When your group Life Insurance coverage ends or reduces, refer to Section 17 for details about converting it to an individual Life Insurance policy.
For Dependent(s) of Active Employees
Your Dependent s coverage will end on the earliest of the following dates:
- the end of the month in which your insurance coverage ends.
- the date the group contract is no longer in force.
- the end of the period for which premiums have been paid for the Dependent coverage.
- the date the Dependent no longer meets the definition of an eligible Dependent.
- the date you die. For Survivor Benefits see Section 10.
Bridging Benefit
Please refer to the bridging benefit provisions under Article 26.06 D of the Academic Collective Agreement and Section 8 of this booklet.
Coverage after Retirement
If you retire, you may be eligible to continue certain benefits. Please request information from your College’s Benefits Administrator or refer to the College Employer Council s website at www.collegeemployercouncil.ca for an explanation of the benefits available to retiring employees.
Section 10 - Survivor Benefits
Survivor Benefits
For Dependent(s) of Active Employees
Provided you are participating in the Dependent coverage for Extended Health Care, Vision Care, Hearing Care and Dental Care when you die, coverage for your Dependents will continue until the earliest of the following dates:
- the last day of the sixth month following the month in which you die, unless the survivor elects to continue the coverage.
- the date the benefit provision under which the Dependent is covered terminates.
- the end of the period for which premiums have been paid.
- the date the group contract terminates.
- the date the survivor would no longer be considered the employee’s dependent if the employee were still alive.
- the date the survivor cancels the coverage.
- the date the survivor dies.
- the end of the month of when you would have reached age 65.
Who pays the premium?
The eligible survivor may elect to continue Extended Health Care, Dental Care, Vision and Hearing Care. The College pays the full premium for the first six months for the Extended Health Care coverage. Beyond six months, the eligible survivor will be required to pay the full premium for the Extended Health Care coverage. The eligible survivor may elect to continue the Vision, Hearing and Dental Care coverage, and is required to pay the College quarterly, in advance, the full cost of the Plans.
Thereafter, the eligible survivor who is in receipt of a lifetime monthly survivor pension, may elect to participate in retirement benefits provided such election is made within 31 days from the end of the month you would have reached age 65 and the eligible survivor continues to be eligible for benefits under OHIP or another Canadian medicare plan equivalent to OHIP from another province or territory.
The eligible survivor will keep the College informed of any change in address or other information as the College or the insurer may require. The eligible survivor will be requested to provide the following information in order to ensure claims are paid appropriately and delays in processing the payments are avoided.
- their date of birth.
- proof that they are in receipt of a lifetime monthly survivor pension from the CAAT Pension Plan or the Teachers Pension Plan.
Section 11 – Extended Health Care (Medicare Supplement)
General description of the coverage
The Extended Health Care Plan pays for eligible services or supplies that are medically necessary for the treatment of an illness and supplements your provincial hospital and medical insurance plans (e.g. OHIP). However, there are additional eligibility requirements that apply to drugs (see Prior authorization program for details). Medically necessary means generally recognized by the Canadian medical profession as effective, appropriate and required in the treatment of an illness in accordance with Canadian medical standards. Any amount payable under the Extended Health Care Plan is subject to the coinsurance and the list of eligible expenses. The Ontario Health Insurance Act prohibits duplication of coverage of the provincial medical and hospital plans. To qualify for this coverage you must be a Canadian resident and entitled to coverage under OHIP, (see also Section 14) or another Medicare plan equivalent to OHIP from another Canadian province or territory or Canadian federal government plan.
In some instances, where permitted by law, expenses covered under this Extended Health Care plan are integrated with certain provincial medicare programs such as the Ontario Assistive Devices Program (ADP) and the Ontario Drug Benefit Plan (ODB). Please refer to the end of Section 13 for a brief description of these programs.
Reference to Doctor may also include a nurse practitioner – If the applicable provincial legislation permits nurse practitioners to prescribe or order certain supplies or services, Sun Life will reimburse those eligible services or supplies prescribed or ordered by a nurse practitioner the same way as if they were prescribed or ordered by a doctor. For drugs, refer to Other health professionals allowed to prescribe drugs.
Who is covered?
All Partial-Load Academic employees who have completed the enrolment form electing the benefit and served the waiting period are covered by the Extended Health Care Plan which includes semi-private hospital accommodation.
Waiting Period
Completion of one calendar month of employment. The coverage begins on the first day of the month following the completion of your waiting period provided you are actively at work on that day. Otherwise the insurance becomes effective when you return to work.
Amount of Coverage
100% of the difference between the cost of a ward and the semi-private hospital room rate in Canada.
85% of eligible expenses for:
- services, while not confined to a hospital, of private duty registered nurses or registered trained attendants, if medically necessary, to an annual maximum of $25,000 per insured individual.
- eligible prescription drugs.
- eligible medical services.
- dental services required as the result of an accident.
- paramedical services.
Payment after coverage ends
If your Extended Health Care Insurance terminates while you are Totally Disabled, treatment of the disabling condition will be covered while your Total Disability continues, as if your insurance under the Plan had continued in force for an additional 6 months.
Coverage under more than one plan
If you are covered for Extended Health Care under another plan, your benefits will be co-ordinated with the other plan following insurance industry standards. Please refer to the ‘Submission of Claim’ section of this booklet for instructions.
Hospital expenses in Canada
Reimbursement Amount
The Plan will cover 100% of the following costs:
- the difference between the cost of a ward and semi-private hospital accommodation, when confined to a hospital in Canada (includes all provinces and territories in Canada).
- hospital out-patient services provided in Canada, except for any services explicitly excluded under this benefit.
Prescription Drugs and Vaccines
Please note that doctors occasionally prescribe drugs which may be readily available over the counter or vaccines that do not require a prescription by law. These drugs and/or vaccines are not covered by the Plan, except as otherwise indicated below under eligible expenses. Ask your pharmacist about the category of the drug you have been prescribed when you get your prescription filled.
For further information or to confirm coverage you may contact Sun Life s call centre at 1-800-361-6212 or 416-753-4300 or by e-mail at askus@sunlife.ca (must have your contract and certificate number available).
Reimbursement Amount
The Plan will cover 85% of the cost of the following drugs and supplies that are prescribed by a licensed doctor or dentist and are obtained from a licensed pharmacist. Drugs covered under this plan must have a Drug Identification Number (DIN) in order to be eligible.
- drugs that legally require a written prescription.
- life-sustaining drugs that may not legally require a prescription.
- injectable drugs and vitamins.
- compounded preparations, provided that the principal active ingredient is an eligible expense and has a DIN.
- diabetic supplies.
- drugs for the treatment of infertility.
- drugs for the treatment of sexual dysfunction.
Drug substitution limit
Charges in excess of the lowest priced equivalent drug are not covered unless the doctor specifies in writing that no substitution for the prescribed drug may be made.
The following items are covered on a reimbursement basis, they are not available with the drug card:
- vaccines that legally require a prescription. However, the Plan also covers hepatitis B and influenza vaccines.
- intrauterine devices (IUDs) and diaphragms.
- colostomy supplies.
- varicose vein injections if medically necessary.
Payments for any single purchase are limited to the cost of a supply that can reasonably be used in a 34 day period or, in the case of maintenance drugs, up to 100 days as ordered by a doctor.
The Plan will not pay for the following, even when prescribed:
- infant formulas (milk and milk substitutes), minerals, proteins, vitamins and collagen treatments.
- the cost of giving injections, serums and vaccines.
- treatments to encourage weight loss, including drugs, proteins and food or dietary supplements.
- hair growth stimulants.
- products to help a person quit smoking.
- over-the-counter drugs, except as otherwise provided under the list of eligible expenses above.
- drugs that are used for cosmetic purposes.
- natural health products, whether or not they have a Natural Product Number (NPN).
- drugs and treatments, and any services and supplies relating to the administration of the drug and treatment, administered in a hospital, on an in-patient or out-patient basis, or in a government-funded clinic or treatment facility.
- drugs and supplies that do not qualify as eligible medical expenses under the Income Tax Act (Canada).
Prior authorization program
The prior authorization (PA) program applies to a limited number of drugs and, as its name suggests, prior approval is required for coverage under the program. If you submit a claim for a drug included in the PA program and you have not been pre-approved, your claim will be declined.
In order for drugs in the PA program to be covered, you need to provide medical information. Please use Sun Life s PA form to submit this information. Both you and your doctor need to complete parts of the form.
You will be eligible for coverage for these drugs if the information you and your doctor provide meets Sun Life’s clinical criteria based on factors such as:
- Health Canada Product Monograph.
- recognized clinical guidelines.
- comparative analysis of the drug cost and its clinical effectiveness.
- recommendations by health technology assessment organizations and provinces.
- your response to preferred drug therapy.
If not, your claim will be declined.
Sun Life’s prior authorization forms are available from the following sources:
- Sun Life’s website at www.mysunlife.ca/priorauthorization
- Sun Life’s Customer Care centre by calling toll-free 1-800-361-6212
Other health professionals allowed to prescribe drugs
The Plan will reimburse certain drugs prescribed by other qualified health professionals the same way as if the drugs were prescribed by a doctor or a dentist if the applicable provincial legislation permits them to prescribe those drugs.
Medical services
Reimbursement Amount
The Extended Health Care Plan will cover 85% of the costs for the medical services listed below when ordered by a doctor (the services of a licensed dentist do not require a doctor s order).
Private Duty Nursing
A pre-determination of eligibility is required for this benefit for you or your dependents. Obtain and submit the In Home Nursing Care Questionnaire form which is to be completed by the attending physician. Expenses for private duty nursing services, outside of a hospital, are eligible if the care is:
- carried out by a registered graduate nurse (R.N.), certified nursing assistant (C.N.A.), registered nursing assistant (R.N.A.), or licensed practical nurse (L.P.N.). Service provider must be licensed, certified or registered in the province where you live and who does not normally live with you.
- medically necessary and prescribed by the licensed attending physician, and
- the type of medical care can only be performed by a qualified R.N., C.N.A., R.N.A., or L.P.N..
- services must be for nursing care and not for custodial care.
Ambulance
OHIP covers the cost of licensed ambulance services, where medically necessary, for local transportation of the person to and from the nearest hospital qualified to provide the required care. You are responsible to pay a co-payment which is currently $45 (subject to change) for these services. The Extended Health Care Plan will reimburse you for 85% of the co-payment amount.
In the event that an unexpected condition occurs (emergency situation) such as illness, disease or injury which requires immediate assistance, the expense for the use of a licensed air ambulance for transportation of the person to the nearest hospital qualified to render the emergency medical services is covered by OHIP in the Province of Ontario. The EHC Plan will pay a maximum of what would have been payable for a local land ambulance trip.
Dental Services as the result of an accident
Dental services for the repair or alleviation of damages to natural teeth sustained in an accident occurring while you or your Dependent(s) are insured under this provision. The services include braces and splints. These services must be received within 12 months after the accident. You will not be covered for more than the fee stated in the Dental Association Fee Guide for a general practitioner in the Province of Ontario. The fee guide must be the current guide at the time that treatment is received.
Note: It will be necessary for you to provide to Sun Life a separate detailed account of the cause of the injury along with the Extended Health Care claim form.
Medical Supplies and Equipment
The Plan covers medically necessary equipment rented that meets the person’s basic medical needs. It is important to note that where the purchase of durable equipment is less expensive than rental, it will be given consideration by Sun Life.
When suitable alternate equipment is available, eligible expenses are limited to the cost of the least expensive equipment that meets the person s basic medical needs. For example, manual wheelchairs are normally considered sufficient to meet basic medical needs, except if the person s medical condition warrants the use of an electric wheelchair.
- casts, splints, trusses, braces and crutches.
- breast prostheses and surgical bras, required as a result of surgery, up to a maximum of $600 per person in any calendar year.
- artificial limbs and eyes (excluding myoelectric and microprocessor appliances) including repairs and replacements when medically necessary.
- oxygen and its administration. Coverage may be co-ordinated with the Assistive Devices Program administered by the Province. Further information is provided at the end of this section.
- wigs required as a result of illness or following chemotherapy.
- elastic support stockings, including pressure gradient hose, up to a combined maximum of 4 pairs per person in a calendar year.
- Continuous Glucose Monitor (CGM) receivers, transmitters or sensors, for persons diagnosed with Type 1 diabetes, up to a combined maximum of $4,000 per person per benefit year. You must provide us with a doctor’s note confirming the diagnosis.
- cannabis for medical treatment, if the information you and your doctor provide on Sun Life’s Prior Approval Form for Medical Cannabis meets clinical criteria, including symptoms, for conditions approved by us. If you submit a claim for medical cannabis and have not been pre-approved, your claim will be declined. Medical cannabis must be dispensed according to Health Canada’s regulations. The maximum amount payable is $4,000 per person per benefit year. To obtain Sun Life s Prior Approval Form for Medical Cannabis, call Sun Life’s Customer Care Centre toll-free at 1-800-361-6212.
Orthopaedic Shoes or Orthotics
Custom-made orthotic inserts for shoes or custom-made orthopaedic shoes or modifications to orthopaedic shoes, when prescribed by a doctor, podiatrist or chiropodist, up to a maximum of 2 pairs for persons under 8 years of age, and one pair for persons 8 years of age and over, in a calendar year.
Paramedical services
The Plan will cover 85% of the costs, up to a combined maximum of $2,000 per insured person in a calendar year for all eligible expenses listed below; this includes the difference between what OHIP allows for podiatrists and your actual charge.
Paramedical services must be deemed by the profession’s licensing/regulatory board to be within the scope of that profession. A service deemed to not be within the scope of the profession will not be covered.
Note: The paramedical service provider must be licensed to practice in the province in which the services are rendered.
Doctor’s order not required:
Services of licensed acupuncturists, audiologist, chiropodist*, chiropractor*, massage therapist, naturopath, occupational therapist, optometrist/ophthalmologist, osteopath (this category of paramedical specialists also includes osteopathic practitioners)*, psychologist, psychotherapist, physiotherapist, podiatrist*, social worker and speech therapist.
*includes one x-ray examination per specialty each calendar year
What is not covered
The Plan will not pay for the costs of:
- services or supplies payable or available (regardless of any waiting list) under any government-sponsored plan or program, except as described below under Integration with government programs.
- services or supplies payable in whole or in part under the provisions of the Medicare Plan in your province of residence.
- hospital services or supplies to the extent they are covered under the Hospital Plan which are paid for in whole or in part under the provisions of the Medicare Plan, whether or not you or your Dependent(s) are enrolled under the provincial plan.
- services or supplies for which the person is eligible for payment under any group medical, surgical or hospital plan.
- any services or supplies that are not usually provided to treat an illness, including experimental or investigational treatments. Experimental or investigational treatments mean treatments that are not approved by Health Canada or other government regulatory body for the general public.
- services or supplies that do not qualify as medical expenses under the Income Tax Act (Canada).
- any services or supplies over the reasonable and customary charges in the locality where they are provided.
The Plan will not pay benefits when the claim is for an illness resulting from:
- the hostile action of any armed forces, insurrection or participation in a riot or a civil commotion.
- any work for which you were compensated that was not done for the College who is providing this Plan.
- the Plan will also not pay benefits when compensation is available under the Workplace Safety and Insurance Act, Criminal Injuries Compensation Act or similar legislation.
Moving Out of Province
If you move from one province to another province or territory it is important that you register for the provincial medicare plan in your new province as soon as possible (90 days or whatever is indicated by the province you are moving to) so that you do not jeopardize your Group Insurance benefits coverage. You are not eligible for Extended Health Care coverage under this plan if you do not have provincial medicare coverage.
Section 12 - Vision Care
Vision Care
To correct a vision impairment, the Plan will cover the cost of contact lenses, laser eye correction surgery or eyeglasses-lenses and frames including tinting, sunglasses, safety glasses and their replacement, as long as they are prescribed in writing by an ophthalmologist or a licensed optometrist and are obtained from an ophthalmologist, licensed optometrist or qualified optician.
Laser eye correction surgery must be performed by an ophthalmologist and may be co-ordinated with available coverage under paramedical services.
Coverage
The Plan will cover 100% of these costs up to a maximum of $400 in any benefit year for persons under 18 years of age, with the benefit year commencing January 1 and a two-year Benefit period for persons 18 years of age and older, with the benefit period commencing January 1, of even numbered years. Maximums will renew annually for persons under age 18 years of age and every 2 years for all other persons.
The Plan will not pay for glasses of any kind purchased over the counter.
Section 13- Hearing care
Hearing Care
To correct a hearing impairment, the Plan will cover hearing aids, including maintenance and repairs, prescribed in writing by an Ear, Nose and Throat (E.N.T.) specialist, Otolaryngologist, Medical Doctor (M.D.) or an Audiologist, up to a maximum of $3,000 per person for the three-year benefit period commencing on January 1, 2022.
In addition to the more usual hearing aid devices, coverage will also include expenses for aids to hearing if prescribed by a medical doctor. These will include:
- a device that produces extra-loud audible signals such as a bell, horn, or buzzer;
- a device to permit the volume adjustment of telephone equipment above normal levels;
- a bone-conduction telephone receiver; and
- the batteries that are required for that purpose, and repairs.;
- teletypewriter or similar device, including a telephone ringing indicator, that enables an individual to make and receive telephone calls;
- a device to decode special television signals to permit the script of a program to be visually displayed; and
- a visual or vibratory signaling device, including a visual fire alarm indicator, for an individual with a hearing impairment.
The above coverage will be subject to the $3,000 maximum per insured person as noted above.
Coverage may be co-ordinated with the Assistive Devices Program administered by the Province.
Coverage Under more than one Plan
If you are covered for Vision or Hearing care under another plan, your benefits will be co-ordinated with the other plan following insurance industry standards. Please refer to the ‘Submission of Claim’ section of this booklet for instructions.
Your coordination with Government Plans
Details of current coverage under the government medicare plans can be found on the website of the Ontario Ministry of Health and Long Term Care at www.health.gov.on.ca. The following provides a brief description of some of the services that are integrated with your Extended Health Care coverage.
Assistive Devices Program (ADP): This program is operated by the Ontario Ministry of Health. It assists Ontario Residents covered by the Ontario Health Insurance Plan who have a long term physical disability (ask your doctor for details). The program covers a number of items such as hearing aids, orthotic devices, ostomy supplies, prosthetic devices (such as breast prostheses), etc. As coverage can change from time to time, please refer to the Ontario Ministry of health and Long Term Care website for details.
Home Oxygen Program (HOP): This program covers oxygen and oxygen delivery equipment such as concentrators, liquid systems, masks, tubing, etc. Contact the Operational Support branch of the Ontario Ministry of Health and Long Term Care for details.
Ontario Drug Benefit Plan (ODB): You and/or your spouse are eligible for the prescription drug benefit on the first day of the month following the attainment of age 65.
Section 14 - Expenses Out Of Your Province and Your Extended Health Care Plan
Expenses out of your province
The Plan will cover emergency services while you are outside the province where you live. The Plan also covers referred services.
For both emergency services and referred services, the Plan will cover the cost of:
- a semi-private hospital room.
- other hospital services provided outside of Canada.
- out-patient services in a hospital.
- the services of a doctor.
Expenses for all other services or supplies eligible under this plan are also covered when they are incurred outside the province where you live, subject to the reimbursement level and all conditions applicable to those expenses.
Emergency services
The Plan will pay 100% of the cost of covered emergency services.
The Plan will only cover emergency services obtained within 60 days of the date you leave the province where you live. If hospitalization occurs within this period, in-patient services are covered until the date you are discharged.
Emergency services mean any reasonable medical services or supplies, including advice, treatment, medical procedures or surgery, required as a result of an emergency. When a person has a chronic condition, emergency services do not include treatment provided as part of an established management program that existed prior to the person leaving the province where the person lives.
Emergency means an acute illness or accidental injury that requires immediate, medically necessary treatment prescribed by a doctor.
At the time of an emergency, you or someone with you must contact Sun Life s Emergency Travel Assistance provider, AZGA Service Canada Inc. (Allianz Global Assistance). All invasive and investigative procedures (including any surgery, angiogram, MRI, PET scan, CAT scan), must be pre-authorized by Allianz Global Assistance prior to being performed, except in extreme circumstances where surgery is performed on an emergency basis immediately following admission to a hospital.
If contact with Allianz Global Assistance cannot be made before services are provided, contact with Allianz Global Assistance must be made as soon as possible afterwards. If contact is not made and emergency services are provided in circumstances where contact could reasonably have been made, then Sun Life has the right to deny or limit payments for all expenses related to that emergency.
An emergency ends when you are medically stable to return to the province where you live.
Emergency services excluded from coverage
Any expenses related to the following emergency services are not covered:
- services that are not immediately required or which could reasonably be delayed until you return to the province where you live, unless your medical condition reasonably prevents you from returning to that province prior to receiving the medical services.
- services relating to an illness or injury which caused the emergency, after such emergency ends.
- continuing services, arising directly or indirectly out of the original emergency or any recurrence of it, after the date that Sun Life or Allianz Global Assistance, based on available medical evidence, determines that you can be returned to the province where you live, and you refuse to return.
- services which are required for the same illness or injury for which you received emergency services, including any complications arising out of that illness or injury, if you had unreasonably refused or neglected to receive the recommended medical services.
- where the trip was taken to obtain medical services for an illness or injury, services related to that illness or injury, including any complications or any emergency arising directly or indirectly out of that illness or injury.
Referred services
Referred services must be for the treatment of an illness and ordered in writing by a doctor located in the province where you live. The Plan will pay 80% of the costs of referred services. Your provincial medicare plan must agree in writing to pay benefits for the referred services.
All referred services must be:
- obtained in Canada, if available, regardless of any waiting lists, and
- covered by the medicare plan in the province where you live.
However, if referred services are not available in Canada, they may be obtained outside of Canada.
Emergency services outside Canada
Expenses incurred for emergency services outside Canada are subject to a lifetime maximum of $2,000,000 per person or, if lower, any other applicable lifetime maximum.
Emergency Travel Assistance
In this section, you means the employee and all dependents covered for Emergency Travel Assistance benefits.
General description of the coverage
If you are faced with a medical emergency when travelling outside of the province where you live, AZGA Service Canada Inc. (Allianz Global Assistance) can help. (Information regarding Allianz Global Assist can be found on the Sun Life Financial Plan Member Services website at www.mysunlife.ca)
Emergency means an acute illness or accidental injury that requires immediate, medically necessary treatment prescribed by a doctor.
This benefit, called Medi-Passport, supplements the emergency portion of your Extended Health Care coverage. It only covers emergency services that you obtain within 60 days of leaving the province where you live. If hospitalization occurs within this time period, in-patient services are covered until you are discharged.
The Medi-Passport coverage is subject to any maximum applicable to the emergency portion of the Extended Health Care benefit. The emergency services excluded from coverage, and all other conditions, limitations and exclusions applicable to your Extended Health Care coverage also apply to Medi-Passport.
We recommend that you bring your Travel card with you when you travel. It contains telephone numbers and the information needed to confirm your coverage and receive assistance.
Getting help
At the time of an emergency, you or someone with you must contact Allianz Global Assistance. If contact with Allianz Global Assistance cannot be made before services are provided, contact with Allianz Global Assistance must be made as soon as possible afterwards. If contact is not made and emergency services are provided in circumstances where contact could reasonably have been made, then Sun Life has the right to deny or limit payments for all expenses related to that emergency.
Access to a fully staffed coordination centre is available 24 hours a day. Please consult the telephone numbers on the Travel card.
Allianz Global Assistance may arrange for:
On the spot medical assistance
Allianz Global Assistance will provide referrals to physicians, pharmacists and medical facilities.
As soon as Allianz Global Assistance is notified that you have a medical emergency, its staff, or a physician designated by Allianz Global Assistance, will, when necessary, attempt to establish communications with the attending medical personnel to obtain an understanding of the situation and to monitor your condition. If necessary, Allianz Global Assistance will also guarantee or advance payment of the expenses incurred to the provider of the medical service.
Allianz Global Assistance will provide translation services in any major language that may be needed to communicate with local medical personnel.
Allianz Global Assistance will transmit an urgent message from you to your home, business or other location. Allianz Global Assistance will keep messages to be picked up in its offices for up to 15 days.
Transportation home or to a different medical facility
Allianz Global Assistance may determine, in consultation with an attending physician, that it is necessary for you to be transported under medical supervision to a different hospital or treatment facility or to be sent home.
In these cases, Allianz Global Assistance will arrange, guarantee, and if necessary, advance the payment for your transportation.
Sun Life or Allianz Global Assistance, based on available medical evidence, will make the final decision whether you should be moved, when, how and to where you should be moved and what medical equipment, supplies and personnel are needed.
Meals and accommodations expenses
If your return trip is delayed or interrupted due to a medical emergency or the death of a person you are travelling with who is also covered by this benefit, Allianz Global Assistance will arrange for your meals and accommodations at a commercial establishment. We will pay a maximum of $150 a day for each person for up to 7 days.
Allianz Global Assistance will arrange for meals and accommodations at a commercial establishment, if you have been hospitalized due to a medical emergency while away from the province where you live and have been released, but, in the opinion of Allianz Global Assistance, are not yet able to travel. We will pay a maximum of $150 a day for up to 5 days.
Travel expenses home if stranded
Allianz Global Assistance will arrange and, if necessary, advance funds for transportation to the province where you live:
- for you, if due to a medical emergency, you have lost the use of a ticket home because you or a dependent had to be hospitalized as an in-patient, transported to a medical facility or repatriated; or
- for a child who is under the age of 16, or mentally or physically handicapped, and left unattended while travelling with you when you are hospitalized outside the province where you live, due to a medical emergency.
If necessary, in the case of such a child, Allianz Global Assistance will also make arrangements and advance funds for a qualified attendant to accompany them home. The attendant is subject to the approval of you or a member of your family.
We will pay a maximum of the cost of the transportation minus any redeemable portion of the original ticket.
Travel expenses of family members
Allianz Global Assistance will arrange and, if necessary, advance funds for one round-trip economy class ticket for a member of your immediate family to travel from their home to the place where you are hospitalized if you are hospitalized for more than 7 consecutive days, and:
- you are travelling alone, or
- you are travelling only with a child who is under the age of 16 or mentally or physically handicapped.
We will pay a maximum of $150 a day for the family member s meals and accommodations at a commercial establishment up to a maximum of 7 days.
Repatriation
If you die while out of the province where you live, Allianz Global Assistance will arrange for all necessary government authorizations and for the return of your remains, in a container approved for transportation, to the province where you live. We will pay a maximum of $5,000 per return.
Vehicle return
Allianz Global Assistance will arrange and, if necessary, advance funds up to $500 for the return of a private vehicle to the province where you live or a rental vehicle to the nearest appropriate rental agency if death or a medical emergency prevents you from returning the vehicle.
Lost luggage or documents
If your luggage or travel documents become lost or stolen while you are travelling outside of the province where you live, Allianz Global Assistance will attempt to assist you by contacting the appropriate authorities and by providing directions for the replacement of the luggage or documents.
Coordination of coverage
You do not have to send claims for doctors’ or hospital fees to your provincial medicare plan first. This way you receive your refund faster. Sun Life and Allianz Global Assistance coordinate the whole process with most provincial plans and all insurers, and send you a cheque for the eligible expenses. Allianz Global Assistance will ask you to sign a form authorizing them to act on your behalf.
If you are covered under this group plan and certain other plans, we will coordinate payments with the other plans in accordance with guidelines adopted by the Canadian Life and Health Insurance Association.
The plan from which you make the first claim will be responsible for managing and assessing the claim. It has the right to recover from the other plans the expenses that exceed its share.
Limits on advances
Advances will not be made for requests of less than $200. Requests in excess of $200 will be made in full up to a maximum of $10,000.
The maximum amount advanced will not exceed $10,000 per person per trip unless this limit will compromise your medical care.
Reimbursement of expenses
If, after obtaining confirmation from Allianz Global Assistance that you are covered and a medical emergency exists, you pay for services or supplies that were eligible for advances, Sun Life will reimburse you.
To receive reimbursement, you must provide Sun Life with proof of the expenses within 30 days of returning to the province where you live. Your employer can provide you with the appropriate claim form.
Your responsibility for advances
You will have to reimburse Sun Life for any of the following amounts advanced by Allianz Global Assistance:
- any amounts which are or will be reimbursed to you by your provincial medicare plan.
- that portion of any amount which exceeds the maximum amount of your coverage under this plan.
- amounts paid for services or supplies not covered by this plan.
- amounts which are your responsibility, such as deductibles and the percentage of expenses payable by you.
Sun Life will bill you for any outstanding amounts. Payment will be due when the bill is received. You can choose to repay Sun Life over a 6 month period, with interest at an interest rate established by Sun Life from time to time. Interest rates may change over the 6 month period.
Limits on Emergency Travel Assistance coverage
There are countries where Allianz Global Assistance is not currently available for various reasons. For the latest information, please call Allianz Global Assistance before your departure.
Allianz Global Assistance reserves the right to suspend, curtail or limit its services in any area, without prior notice, because of:
- a rebellion, riot, military up-rising, war, labour disturbance, strike, nuclear accident or an act of God.
- the refusal of authorities in the country to permit Allianz Global Assistance to fully provide service to the best of its ability during any such occurrence.
Liability of Sun Life or Allianz Global Assistance
Neither Sun Life nor Allianz Global Assistance will be liable for the negligence or other wrongful acts or omissions of any physician or other health care professional providing direct services covered under this group plan.
Section 15 - Dental Plan
General description of the coverage
Amount of Coverage
- 100% of eligible expenses for preventative dental procedures.
- 100% of eligible expenses for restorative and surgical procedures.
- 100% of eligible expenses for prosthodontic procedures.
- 50% of eligible expenses for inlays, onlays, crowns, repairs of crowns, repair of bridges, construction and insertion of bridges.
- 50% of eligible expenses for orthodontic procedures.
What are the maximums?
| Insured Percentage | Maximum | |
|---|---|---|
| Types A, B and C Basic Services, including dentures | Types A, B and C Basic Services, including dentures Insured Percentage: 100% | Types A, B and C Basic Services, including dentures Maximum: $2,500 each calendar year for Types A, B and C combined |
| Type E Crowns & Bridges | Type E Crowns & Bridges Insured Percentage: 50% | Type E Crowns & Bridges Maximum: $2,500 each calendar year |
| Type D Orthodontic | Type D Orthodontic Insured Percentage: 50% | Type D Orthodontic Maximum: $2,500 (Lifetime) |
What fees are covered?
The fees stated in the Ontario Dental Association Fee Guide for general practitioners which was current one year prior to the date the eligible expenses were incurred, regardless of where the treatment is received. The specific Ontario Dental Association procedure codes for the services described below are posted on the Council’s website at www.collegeemployercouncil.ca and are subject to change from year to year.
Temporary Dental Services
If you receive any temporary dental service, it will be included as part of the final dental procedure used to correct the problem, and not as a separate procedure.
Preventive Dental Procedures
(Type A – 100%)
Your dental benefits cover procedures used to help prevent dental problems including:
Oral examinations
- initial examination every 24 months.
- 1 recall examination every 5 months, up to a maximum of 2 examinations per calendar year.
- emergency or specific examinations.
- preventive recall packages.
X-rays
- 1 complete series of x-rays or 1 panorex every 24 months.
- 1 set of bitewing x-rays every 6 months, up to a maximum of 2 sets per calendar year.
- X-rays to diagnose a symptom or examine progress of a particular course of treatment.
Other services
- Required consultations with another dentist, excluding those for orthodontic purposes.
- Required consultations between the patient and dentist, excluding those for orthodontic purposes.
- Fillings – amalgam, silicate, composite, acrylic or equivalent.
- Polishing (cleaning) and topical fluoride treatment, once every 6 months, up to a maximum of 2 per calendar year.
- Protective athletic appliance (mouthguards).
- Scaling.
- Other preventive services.
- Diagnostic tests and laboratory examinations, but excluding x-rays, study models or similar records prepared for orthodontic procedures.
- Provision of space maintainers for missing primary teeth.
Restorative Dental and Surgical Procedures
(Type B 100%)
Your dental benefits include procedures used to treat basic dental problems and include:
Required consultation between your Dentist and another Dentist.
Retentive pins.
Prefabricated, full coverage restorations.
Caries, trauma and pain control.
Professional visits.
Extraction of teeth
- Removal of teeth.
Endodontics
- Root canal therapy and root canal fillings, and treatment of disease of the pulp tissue.
Periodontics
- Treatment of disease of the gum and other supporting tissue.
Oral surgery
- Surgery and related anaesthesia, other than implants, transplants and repositioning of the jaw.
- Therapeutic intra-muscular or intravenous drug injection.
- Adjunctive general services.
Denture Procedures
(Type C – 100%)
Your dental benefits include removable dental prosthesis to resolve dental problems and include:
- Complete maxillary and/or mandibular dentures – once every 3 years per arch.
- Removable partial dentures – once every 3 years.
- Denture adjustments.
- Repair of dentures.
- Rebase or reline of an existing partial or complete denture.
- Customary commercial laboratory fees associated with the above.
Crowns and Bridges
(Type E – 50%)
Your dental benefits include permanent dental prosthesis to resolve dental problems and include:
- Bridges.
- Repairs to bridges.
- Inlays
- Onlays
- Pins in inlays, onlays and crowns
- Post and core
- Crowns and repairs to crowns.
[Special Provisions for Implants: If a claim is made for an implant, the implant itself and related surgery are not an eligible expense under the Plan; however, the plan may reimburse you for up to the level of service that is applicable under the alternate benefit clause.
The Plan will pay based on the least expensive alternate service as follows:
- If a crown is the least expensive alternate service, the Plan will reimburse the allowable fee for a standard crown.
- If a denture is the least expensive alternate service , the Plan will reimburse up to the allowable fee for a denture, either partial or full.
- If a bridge is the least expensive alternate service , the Plan will reimburse up to the allowable fee for a bridge.
Please refer to the section “What is not covered” for more information about the alternate benefit clause. A pre-determination will identify what portion of the cost, if any, will be reimbursed.]
Replacement of dentures and bridges
Charges for a replacement bridge or replacement standard dentures are not considered an eligible expense during the 3 year period following the construction or insertion of its predecessor except where:
- it is needed to replace a bridge or standard denture which has caused temporomandibular joint disturbances and which cannot be economically modified to correct the condition, or
- it is needed to replace a transitional denture which was inserted shortly following extraction of teeth and which cannot be economically modified to the final shape required.
Orthodontic Procedures
(Type D – 50%)
Your dental benefits include procedures used to treat misaligned and crooked teeth and include:
Coverage includes orthodontic examinations, including orthodontic diagnostic services and fixed or removable appliances such as braces.
The following orthodontic procedures are covered:
- Required consultations between patient and dentist
- Diagnostic services – orthodontic cast.
- Observation and adjustment.
- Repairs.
- Alterations.
- Re-cementations.
- Separation.
- Fixed – bilateral/unilateral or removable orthodontic appliances.
- Appliances to control oral habits.
- Myofunctional therapy.
- Retention appliances.
Predetermination
Recommended where expenses will exceed $300
To ensure that you and your Dentist are aware of the expenses that will be paid by the Plan it is strongly recommended that you send a predetermination form to Sun Life, before the work is done, for any major treatment or any procedure.
How do I file a predetermination?
This can be done by your Dentist directly via electronic submission or if necessary:
- you can obtain a claim from your Human Resources Department.
- ask your Dentist to complete the appropriate sections of the form.
- you complete your sections of the form, sign it and forward it to Sun Life.
Sun Life will advise you how much of the planned treatment is covered by the Plan taking into account any possible alternate procedure or course of treatment based on accepted dental practice, and how much of the cost you will be responsible for before the work is done.
Laboratory Fees
- Certain procedures will usually involve the cost of a commercial laboratory and when appropriate, a reasonable and customary laboratory fee will be reimbursed subject to the same overall maximums. Please note that predetermination cannot take laboratory fees into account but the appropriate payment will be included at the time of claim.
The only circumstance in which benefits will be considered for an ineligible procedure is when your Dentist advises, in writing, that it is both less expensive and better for you than the eligible procedure.
Coverage under more than one plan
If you are covered for Dental Care under another plan, your benefits will be co-ordinated with the other plan following insurance industry standards. These standards determine where you should send a claim first. Please refer to the ‘Submissions of Claims’ section of this booklet for instructions.
What is not covered
The Plan will not pay for:
- services or supplies payable or available (regardless of any waiting list) under any government-sponsored plan or program unless explicitly listed as covered under this benefit.
- services or supplies that are not usually provided to treat a dental problem, including experimental treatments.
- any portion of the charge over the usual, customary and reasonable charge of the least expensive alternate service or material consistent with adequate dental services when such alternate service or material is customarily provided.
- procedures performed primarily to improve appearance.
- the replacement of dentures that are lost, misplaced or stolen.
- charges for appointments that you do not keep.
- charges for completing claim forms.
- expenses related to services or supplies of the type normally intended for home use.
Dental expenses resulting from:
- the hostile action of any armed forces, insurrection or participation in a riot or civil commotion.
- commission or attempted commission of a criminal offence by the insured person.
- any cause for which compensation is available under the Workplace Safety and Insurance Act, Criminal Injuries Compensation Act or similar legislation.
Payment After coverage ends
If your coverage terminates, you will still be covered for procedures to repair natural teeth damaged by an accidental blow if:
- the accident occurred while you were still covered, and
- the procedure is performed within 6 months after the date of the accident.
Expenses Outside of Province/Canada
Expenses for emergency dental care outside Canada will qualify as eligible expenses to the extent that they represent the usual, customary and reasonable charges for dental care in the locality where the dental care is performed, provided an expense for such dental care would qualify as an eligible expense, in the Province of Ontario.
For expenses incurred for dental care performed outside Canada on an other than emergency basis, the benefit provided under this contract will be the usual, customary and reasonable charges for dental care in the locality where the dental care is performed but not exceeding the level of eligible expenses for the Province of Ontario.
Section 16 – Short Term Disability Plan (STD)
General description of the coverage
The Colleges have full legal and financial liability for this benefit. Questions or inquiries in regard to this benefit must be directed to your College s Benefits Administrator.
The Short Term Disability Plan (STD) is not an insurance plan. It is a benefit paid directly to you by the College. The full description of the STD Plan is set out in Article 17, 21.07 D and 26.08 of the current Academic Collective Agreement.
Cumulative Sick Leave Credits
A member of the Academic Bargaining Unit employed by the College on a Partial-Load basis on or after April 1, 1991, will accumulate sick leave credits in hours as set out in Article 26.08 B of the current Academic Collective Agreement.
Unused sick leave credits will be accumulated. However, no gratuity entitlement will be attached to these credits.
A member of the Academic Bargaining Unit employed by the College on a Partial-Load basis prior to April 1, 1991, will accumulate sick leave credits as set out in Article 26.08 B of the current Academic Collective Agreement.
Unused sick leave credits will be accumulated. After ten years of service at a single College, any unused sick leave credits are payable upon death, termination or retirement. The formula for calculating payment is:
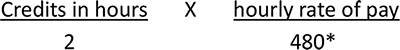
*Annual teaching maximum.
The payout is subject to a maximum gratuity of 50% of the annual maximum number of hours of teaching
(i.e. 10 months X 4 weeks X 12 hours)
Bridging Benefit
The Bridging Benefit is set out in Article 26.08 C of the current Academic Collective Agreement and it applies if you are:
- rehired within 6 months of the end of any contract;
- if upon termination of a contract you have a written contract for future employment as a partial-load employee; or
- you are on an approved leave of absence.
Section 17 - Life Insurance Coverage
General description of the coverage
(Optional)
You may elect to enrol in the Employee Life Insurance benefit. It is term insurance that covers you 24 hours per day while you continue to meet the eligibility requirements for insurance under the group contract. There are three levels of coverage. They are described below.
Basic Life Insurance
If you have elected this insurance you have coverage in the amount of $25,000.
Supplementary Life Insurance
You may choose additional coverage in units of $10,000 up to a maximum of $60,000.
Employee Pay-All Life Insurance
Provided you have chosen the maximum of $60,000 under the Supplementary Life Insurance benefit you may choose to be covered in units of $10,000 up to an additional $300,000 under the Employee Pay-All Life Insurance.
If you are covered for the maximum benefits available under the Plan you would be insured for a total of $385,000.
Change without evidence of insurability
No medical examination or other evidence of insurability is required provided you are actively at work and you apply for the optional life insurance for you or your spouse within 31 days of the following:
- the date you completed your Waiting Period, or
- the date you acquire a Dependent or an additional Dependent, or
- the date your marital status changes.
What happens if I do not apply within 31 days or I wish to increase the amount of Life Insurance?
You will be required to furnish evidence of insurability to Sun Life. Such insurance coverage will take effect only upon the date your evidence of insurability is approved by Sun Life. It is important to note that it is possible that coverage could be declined. Serious consideration should be given before declining the life benefits at the time the benefits are first offered to you.
Coverage during total disability (The contract holder has the sole legal and financial liability for the Coverage during total disability. Sun Life only acts as administrator on behalf of the contract holder)
If you become totally disabled before you retire or reach age 65, whichever is earlier, Life coverage for you and your dependents may continue without the payment of premiums as long as you are totally disabled. This continued coverage is subject to the terms of the contract which were in effect on the date you became totally disabled, including reductions and terminations. In addition, all continued coverage with Sun Life terminates on the date the benefit under which the person is covered with Sun Life terminates.
Sun Life must receive proof of your total disability within 12 months of the date the disability begins. After that, we can require ongoing proof that you are still totally disabled.
If proof of total disability is approved after an individual insurance policy becomes effective as a result of converting the group Life coverage, the group Life coverage will be reduced by the amount of the individual insurance policy, unless the individual insurance policy is exchanged for a refund of premiums.
Total disability must continue for:
- an uninterrupted period of 6 months, or
- the elimination period for Long-Term Disability if you are entitled to Long-Term Disability payments, whichever is shorter.
This coverage will continue without payment of premiums, from the date total disability begins, until the date you cease to be totally disabled or the date you fail to give Sun Life proof of your continued total disability, whichever is earlier.
For the purposes of your Life coverage, you will be considered totally disabled if you are prevented by illness from performing any occupation you are or may become reasonably qualified for by education, training or experience. However, if you are totally disabled under the Long-Term Disability benefit, you are also considered to be totally disabled under the Life benefit.
Accidental Death and Dismemberment
General description of the coverage (Mandatory only if you elect Basic Life Insurance)
Accidental Death and Dismemberment (AD & D) insurance is provided. This means that if, due to an accident occurring while covered, you die or suffer a dismemberment as listed in the table under Table of Losses, you may be eligible for benefits. Any death benefit paid under this coverage is in addition to the Basic Life Insurance coverage.
Accident
An accident is a bodily injury that occurs solely as a direct result of a violent, sudden and unexpected action from an outside source.
Your Accidental Death and Dismemberment Insurance
Amount of Insurance – $25,000
100% of the insurance is payable in the event of accidental death. For other Dismemberment situations the amount payable is $25,000 pro-rated in proportion to the percentages identified in the Table of Losses Chart.
What the Plan will pay
The Plan will pay for this benefit if you:
- accidentally drown.
- disappear in an accident while travelling. This only applies if the means of transportation disappears, sinks, is wrecked, forced to land or stranded and the body is not found within one year. There must be no evidence that you or your spouse are still alive.
- are in an accident or exposed to the elements and, as a direct result, you suffer one of the losses listed below within 365 days of that accident or exposure.
The amount that the Plan will pay is a percentage of the $25,000. The percentage depends on the loss suffered. The following table shows the percentages used to determine the payment. However, only the largest percentage is paid for injuries to the same limb resulting from the same accident, and the maximum payable due to any one accident is $25,000.
TABLE OF LOSSES CHART
| Loss of life | 100% |
|---|---|
| Loss of both hands | 100% |
| Loss of both feet | 100% |
| Loss of one hand | 50% |
| Loss of one foot | 50% |
| Loss of thumb and index finger on the same hand | 33.33% |
| Loss of use of one arm and one leg | 100% |
| Loss of use of one arm | 50% |
| Loss of use of one leg | 50% |
| Loss of entire sight of one eye | 50% |
| Loss of entire sight of both eyes | 100% |
| Loss of sight of one eye and either one hand or one foot | 100% |
Accidental Loss
- Loss of a hand means that it was severed at or above the wrist.
- Loss of a foot means that it was severed at or above the ankle.
- Loss of a thumb and index finger means that they were severed at or above the first joint from the hand.
- Loss of sight must be total and permanent.
Loss of use of limb must be total, continuous for 12 months, and then must be determined to be permanent and irrecoverable before the benefit is payable.
What is not covered
The Plan will not pay AD & D benefits for losses that are the result of:
- suicide or self-inflicted injury, regardless of whether the person has a mental illness or intends or understands the consequences of their actions.
- taking any poison, drug or medicine, whether voluntarily or otherwise.
- inhaling gas, whether voluntarily or otherwise, other than as a result of performance by the employee of the regular duties of his employment.
- bodily or mental infirmity or disease of any kind or infection other than infection occurring simultaneously with and in consequence of an accidental cut or wound.
- flying in, descending from or being exposed to any hazard related to an aircraft while
- receiving flying lessons.
- performing any duties in connection with the aircraft (except when such duties are being performed as part of your occupation with the College).
- being flown for a parachute jump.
- a member of the armed forces if the aircraft is under the control of or chartered by the armed forces.
- war, insurrection or the hostile action of the armed forces of any country.
- participation in a criminal offence
Coverage during total disability
If you became totally disabled while insured, your Accidental Death and Dismemberment coverage will be continued until the end of the month in which you reach age 65.
Dependent Life Insurance Coverage
General description of the coverage
(Optional)
Dependent Life Insurance is term insurance which covers your spouse and dependent children while you remain an employee of the College and they continue to meet the eligibility requirements for the insurance.
Amount of Insurance
Spouse: $5,000 Each child: $2,000
The benefit is payable to you. Its purpose is to assist you and your family with the additional financial burden should your spouse or dependent children die.
Proof of good health
Required on all amount of coverage unless requested within 31 days of completing the waiting period or of acquiring a new dependent.
Coverage during Total Disability
If you became totally disabled while insured, your Dependent Life coverage will be continued until the end of the month in which you reach age 65.
Sun Life must receive proof of your total disability within 12 months of the date the disability begins.
Appointing a Beneficiary
Beneficiary Appointments
You may name the beneficiary of your choice, a person, persons or your estate. In the event of your death, benefits will be paid in the name of the last legally nominated beneficiary designation that you made on mysunlife.ca or you have on file with your Human Resources Department. In the absence of a beneficiary appointment, payment will be made to your estate.
Appointment of a Beneficiary in the Province of Ontario
Except as restricted by law you may change your beneficiary at any time. In the Province of Ontario, the beneficiary is revocable by the insured. This means that you may change your beneficiary appointment at any time without the approval of your beneficiary.
Appointment of a Beneficiary in the Province of Quebec
The Province of Quebec requires that you indicate whether your beneficiary is revocable or irrevocable at the time you make your benefit election. If you have indicated the beneficiary is irrevocable at the time of enrolment, you may only change the beneficiary appointment with the written permission of the current beneficiary. The enrolment form provided by the College contains this information.
Your beneficiary appointment can be a complex matter, and depending on your specific situation, you may wish to seek legal advice before making a nomination and/or changing an appointment. You can sign in to review and update your beneficiary designation on mysunlife.ca or obtain the necessary form from your Human Resources Department.
Life Insurance Conversion
Converting your Life Insurance
While the Life Insurance benefit is in effect with Sun Life, you may apply to convert the group Life coverage, to an individual Life policy with Sun Life without providing proof of good health
It is your responsibility to initiate an application to convert your Life Insurance with Sun Life. The College will issue a conversion form to you. This form will confirm details of your employment such as your start date with the College, the amount of insurance coverage in effect at the time of your separation from the College, the termination date of your insurance as well as providing a list of Sun Life numbers where you can call to get more information about your options on an individual policy. You have 31 days from the date your insurance is reduced or ceases to convert your Life Insurance to an individual Life policy with Sun Life.
You may only exercise the conversion option once.
How much can I convert
You may convert your total Life Insurance coverage to a maximum of $200,000.
If you die during the Conversion Period
If you die during this 31 day conversion period, the conversion amount of Life Insurance coverage will be paid to your last named beneficiary as recorded on your file in the Human Resources Department as a death claim.
Converting your Dependent Life Insurance
While the Dependent Life Insurance benefit is in effect with Sun Life, you may apply to convert your spouse’s Life coverage to an individual Life policy with Sun Life without providing proof of good health. This is not available for dependent children.
How long do I have to convert my spouse’s life insurance?
You have 31 days from the date your Dependent Life insurance ceases to convert to a private policy with Sun Life.
What happens if my spouse dies during the conversion period?
If your Spouse dies during this 31 day conversion period, the conversion amount of Dependent Life Insurance coverage will be paid as a death claim to you.
Section 18 – Critical Illness Insurance
General Description of Coverage
Critical Illness insurance provides protection that Long Term Disability, Life Insurance, and Extended Health Care insurance coverages do not. Following the diagnosis of a critical illness and a prescribed survival period, this insurance pays a one-time, lump-sum benefit (see Critical Illness brochure for additional information).
Eligibility
You are eligible to apply for coverage for yourself and/or your spouse provided you are a Partial-Load Academic employee of the Colleges of Applied Arts and Technology.
To qualify, you must:
- be between the ages of 18 and 69
- reside in Canada
- be actively at work
- provide proof of good health
Eligibility Date
Is the date following the completion of the Waiting Period of one continuous month of Partial-Load employment.
Coverage
Coverage is available to you and your spouse up to a maximum of
$200,000 in units of $25,000.
Coverage Effective Date
- If you and your spouse apply on your Eligibility Date (or prior to), any amount of coverage that does not require medical information $50,000 or less) will be effective on your Eligibility Date.
- If you and your spouse apply within 31 days following your Eligibility Date, any amount of coverage that does not require medical information ($50,000 or less) will be effective on the date the application form was signed. Your Human Resources Department must be in receipt of your signed application form within the 31 days following your Eligibility Date for coverage to be effective.
- If you apply for amounts that exceed $50,000 during your eligibility period, you will be required to complete a medical questionnaire. If approved, you will be notified by Sun Life of the date your coverage will be effective.
- If you apply for coverage after your 31-day eligibility period, medical information will be required for all amounts of coverage applied for.
Insured Critical Illness Conditions
The Colleges of Applied Arts and Technology Critical Illness insurance plan covers a broad range of conditions – 25 in total – as follows:
- Cancer
- Heart Attack (Myocardial Infarction)
- Stroke
- Aorta surgery
- Major organ transplant
- Major burns
- Major organ failure requiring transplant
- Kidney Failure
- Alzheimer’s disease
- Loss of speech
- Parkinson’s disease
- Coronary artery bypass surgery
- Blindness
- Multiple Sclerosis
- Loss of independent existence
- Deafness
- Paralysis
- Coma
- Benign brain tumour
- Occupational HIV Infection
- Aplastic anemia
- Bacterial meningitis
- Heart valve replacement or repair
- Loss of limbs
- Motor neuron disease
For further description of these disabilities please read the “Critical Illness Insurance” brochure.
Limitations and Exclusions
- No benefits are payable for claims resulting from:
- Declared or undeclared war, insurrection or rebellion
- Voluntary participation in a riot or act of civil disobedience
Attempted suicide, or intentionally self-inflicted injuries regardless of whether the person has a mental illness or intends or understands the consequences of their actions - Committing or attempting to commit a criminal offence
- Use of illegal or illicit drugs or substances, misuse of drugs or alcohol
- Any symptom or medical problem leading to a diagnosis or surgery if that symptom or medical problem began or occurred before the first premium due date
- Any symptom or medical problem, leading to a diagnosis of cancer, which commenced within 90 days following the first premium due date
- Death during the required survival period
- For any coverage that does not require health information ($50,000 or less), no benefit is payable for any covered condition that occurs within 12 months after the effective date of the insured person’s coverage, and that resulted from any injury, sickness or medical condition (whether or not diagnosed) for which, during the 12 months prior to the effective date of insurance, the insured person:
- had symptoms
- consulted a physician or other health care practitioner, or
- was provided any health-related care, advice or treatment, or that a reasonable prudent person, with such injury, sickness or medical condition, would have consulted a physician or any other health care practitioner.
Coverage Ends
Your Critical Illness Insurance coverage will end on the earliest of:
- the day you retire;
- the day you reach age 70;
- the date you no longer a resident of Canada;
- the day the benefit is paid for the first covered condition;
- the day your employment ends;
- the day the group contract ends;
- the end of the period for which premiums have been paid; or
- the day of your death.
Your Spouse’s Critical Illness coverage will end on the earlier of:
- the day your spouse no longer qualifies under the definition;
- the day you or your spouse reach age 70;
- the day your spouse no longer resides in Canada;
- the day the benefit is paid for the first covered condition;
- the day your employment ends;
- the day the group contract ends;
- the end of the period for which premiums have been paid; or
- the day of your death or the day of your spouse’s death.
Coverage Conversion
If you lose your Critical Illness insurance coverage through a change in employment, marital status or retire, you and/or your spouse can maintain your coverage up to a maximum of $100,000 by calling Sun Life Financial within 60 days of loss of coverage. If you reach age 65, therefore your coverage terminates, your spouse is still eligible to convert their coverage (up to a maximum of $100,000) if they are under the age of 65.
Note: Not eligible to convert coverage after age 65.
How to Apply
To apply for coverage, contact your College’s Benefits Administrator to obtain an enrolment package.
Section 19 - Submission of Claims
Making Claims
Sun Life is dedicated to processing your claims promptly and efficiently. You should contact your employer to get the proper form to make a claim.
There are time limits for making claims. These limits are discussed in the appropriate sections of this employee benefits booklet. If you fail to abide by these time limits, you may not be entitled to some or all benefit payments.
All claims must be made in writing on forms approved by Sun Life.
For the assessment of a claim, Sun Life may require medical records or reports, proof of payment, itemized bills, or other information Sun Life considers necessary. Proof of claim is at your expense.
Legal Actions
Limitation period for Ontario:
Every action or proceeding against an insurer for the recovery of insurance money payable under the contract is absolutely barred unless commenced within the time set out in the Limitations Act, 2002.
Limitation period for any other province:
Every action or proceeding against an insurer for the recovery of insurance money payable under the contract is absolutely barred unless commenced within the time set out in the Insurance Act or other applicable legislation of your province or territory.
Making an Extended Health Care Claim
Drug Card Plan
The drug card is used for prescription drugs only. The card is accepted at most drug stores across Canada. The drug card cannot be used outside Canada. Other claims, such as physiotherapy or medical supplies, are not covered under the drug card plan and receipts must be submitted to Sun Life using the Extended Health Care claim form to obtain reimbursement. These claims must be submitted to Sun Life using the Extended Health Care claim form.
What happens if I do not use the drug card to purchase my drugs
If you do not use the card for all your drug purchases, your reimbursement could be affected due to pharmacy mark-ups on the cost of the drugs. This means that you may have to pay more out-of pocket
Time limits for filing a claim
- Claims must be received by Sun Life within the earliest of:
548 days following the date on which the expense was incurred, - 90 days following the end of your Extended Health Care coverage, or
- 90 days following the termination of the Extended Health Care provision.
Co-ordination of benefits
(Coverage under more than one plan)
If you are covered for Extended Health Care under this plan and you and or your spouse are covered under another plan, your benefits will be co-ordinated with the other plan following insurance industry
standards.
These standards determine where you should send a claim first. Here are some guidelines:
- if you are claiming expenses for your spouse who is covered for those expenses under another plan, you must send the claim to your spouse’s plan first.
- if you are claiming expenses for your children and both you and your spouse have coverage under different plans, you must claim under the plan of the parent with the earlier birthday (month and day) in the calendar year. For example, if your birthday is May 1 and your spouse’s birthday is June 5, you must claim under your plan first.
- the maximum amount that you can receive from all plans for eligible expenses is 100% of actual expenses.
- If your spouse is over age 65 and eligible for coverage under the Ontario Drug Benefit Program (ODB), there are specific rules to follow. Contact your College’s Benefits Administrator for further details.
Ontario Assistive Devices Program
The Ontario Assistive Devices Program (ADP), run by the Ontario Ministry of Health, helps people who have long-term physical disabilities get needed equipment and supplies. To find out more about this program, contact the Assistive Devices Branch of the Ministry of Health.
The Claims Process
Contacting Sun Life
Private Duty Nursing Claims
Medical Supplies and Equipment
How long will it take for my claim to be processed?
Following up on a claim
How do I make a claim for survivor’s benefits?
Out-of-Province Claims
OHIP first
- your claim for expenses incurred outside the province must be submitted to OHIP first.
- original receipts should be included with your claim and you must keep a copy for your records and/or later submission to Sun Life.
Sun Life second
- the balance of the claim not paid by OHIP should be submitted to Sun Life, using the normal claim form for your Group.
- the OHIP reimbursement statement and copies of your receipts should be attached to the Sun Life claim form.
- be sure to keep a copy of the information sent to Sun Life for your records.
Making a Dental Claim
Time limits for filing a claim
- the end of the calendar year following the year during which you incur the expenses.
- 90 days after the end of your Dental Care coverage.
- 90 days following termination of the Dental Care provision.
Co-ordination of benefits
(Coverage under more than one plan)
The Claims Process
- Ask your Dentist to complete the applicable sections of the claim form.
- You complete the applicable sections of the claim form, sign it, attach any relevant information, and forward it to the Sun Life claims office. The appropriate address is noted on the claim form.
- Keep a copy of the claim form and your receipts for future reference.
- If your Dentist is submitting the claim electronically:
- Your Dentist is required to complete the applicable sections of the claim form.
- You complete the applicable sections of the claim form and sign it.
- Your Dentist electronically forwards the claim directly to Sun Life and the payment is generated immediately. If you have assigned payment to the dentist, payment will be made directly to the Dentist. If payment is to be made to you and you have set up a direct deposit with Sun Life (www.mysunlife.ca) the payment will be deposited to your account within a couple of days. Otherwise, a cheque will be mailed to your home address.
Orthodontic Claims
How long will it take for my claim to be processed?
Following up on a claim
Contacting Sun Life
Making a Life Insurance Claim
Your Death Claim
- A claim form must be completed by the College.
- A claim form must be completed by your beneficiary.
- The completed claim forms along with a death certificate from your attending physician or funeral home must be forwarded to Sun Life in order for the claim to be adjudicated.
For Accidental Death & Dismemberment Claims (Applicable only to employees)
- A claim form must be completed by the College.
- A claim form must be completed by you.
- The completed claim forms along with an Attending Physician’s Statement clearly indicating the date and details of the accident, the nature of the injury, the date of loss and the degree of loss must be forwarded to Sun Life in order for the claim to be adjudicated.
Death Claim for your Dependent(s)
- A claim form must be completed by the College.
- A claim form must be completed by you.
- The completed claim forms along with a death certificate from
- your Dependent’s attending physician or funeral home must be forwarded to Sun Life in order for the claim to be adjudicated.
Making a Critical Illness Insurance Claim
How to make a claim
Your Critical Illness Claim
- a claim form must be completed by you
- the completed claim form along with supporting medical evidence must be forwarded to Sun Life in order for the claim to be adjudicated
Respecting your privacy
Respecting your privacy is a priority for the Sun Life Financial group of companies. We keep in confidence personal information about you and the products and services you have with us to provide you with investment, retirement and insurance products and services to help you meet your lifetime financial objectives. To meet these objectives, we collect, use and disclose your personal information for purposes that include: underwriting; administration; claims adjudication; protecting against fraud, errors or misrepresentations; meeting legal, regulatory or contractual requirements; and we may tell you about other related products and services that we believe meet your changing needs. The only people who have access to your personal information are our employees, distribution partners such as advisors, and third-party service providers, along with our reinsurers. We will also provide access to anyone else you authorize. Sometimes, unless we are otherwise prohibited, these people may be in countries outside Canada, so your personal information may be subject to the laws of those countries. You can ask for the information in our files about you and, if necessary, ask us in writing to correct it. To find out more about our privacy practices, visit www.sunlife.ca/privacy.
You have a choice
We will occasionally inform you of other financial products and services that we believe meet your changing needs. If you do not wish to receive these offers, let us know by calling 1-877-SUN-LIFE (1-877-786-5433).
